Meeko the calf stood nuzzling a pile of hay. He didn’t seem to have much appetite, and he looked a little bored. Every now and then, he glanced up, as though wondering why so many people with clipboards were standing around watching him.
Fourteen hours earlier, I’d watched doctors lift Meeko’s heart from his body and place it, still beating, in a plastic dish. He looked no worse for the experience, whisking away a fly with his tail as he nibbled, demonstrably alive—though above his head, a monitor showed a flatlined pulse. I held a stethoscope to his warm, fragrant flank and heard, instead of the deep lub-dub of a heartbeat, what sounded like a dentist’s drill or the underwater whine of an outboard motor. Something was keeping Meeko alive, but it was nothing like a heart.
As many as five million Americans suffer some form of heart failure, but only about 2,000 hearts a year become available for transplant. The obvious solution to that scarcity is to build an artificial heart, and how hard could that be? The heart’s just a pump, after all, and people have been making pumps since the Mesopotamians invented the shadoof to raise river water 3,000 years before the birth of Christ. Doctors started thinking seriously about replacing the heart with a machine around the time Harry Truman was president.
To understand why they still haven’t succeeded, pick up a two-pound barbell and start curling it. Two pounds: nothing. But see how long you can keep it up. Twenty minutes? An hour? Two? Your heart does that all day and all night—35 million beats a year—for as long as you live, without ever taking a rest. Manufacturing a metal and plastic heart capable of beating that way for more than about 18 months has so far proved impossible.
The problem is the “beating” part. Among the first to envision an artificial heart was, amazingly, the ventriloquist Paul Winchell. When not in front of a TV camera manipulating his dummies Jerry Mahoney and Knucklehead Smiff, Winchell was developing patents, some 30 in all, including one for an artificial heart that he invented with Dr. Henry Heimlich, of the eponymous anti-choking maneuver. Back then, and up through the famous Jarvik-7—the first machine to replace a human heart, in 1982, albeit briefly—inventors could only imagine imitating the heart’s lub-dub.
It turns out that imitating a beating heart with metal and plastic has several limitations. First, the Jarvik-7 and its successors that are still in use require an air compressor outside the body. Through hoses that pierce the skin, the compressor fills a balloon inside one of the Jarvik’s chambers, pushing blood to the lungs. Then it fills a second balloon in another chamber to push blood back out to the body. The two balloons inflate and deflate in an alternating rhythm. It works, but it also means that a patient has to sit beside a big, noisy compressor 24 hours a day. That’s better than dying of heart failure, but it doesn’t make for a great quality of life. Barney Clark, the first person to live entirely on a Jarvik-7, asked his doctors several times, during his 112 days on the device, to let him die.
Twin Turbines
Clark probably would not have been able to hang on much longer in any case. Those balloons, and all other moving parts in a beating mechanical heart, wear out quickly. That’s why, almost 30 years after the first Jarvik-7, artificial hearts remain what is delicately termed “bridges to transplant”—something to keep you alive until a real heart can be found.
A transplantable heart, alas, is an increasingly rare find. It has to come from a person who is in the blush of good health and also, somehow, dead. As cars have gotten safer and states have passed laws requiring seatbelts and motorcycle helmets, the number of such hearts has dwindled. The need for hearts, on the other hand, has grown with the world’s population and the conquering of other diseases. And even when a heart is found, patients face the risk of tissue rejection.
Building a heart that mimics nature’s lub-dub may be as comically shortsighted as Leonardo da Vinci designing a flying machine with flapping wings. Nature is not always the best designer, at least when it comes to things that humans must build and maintain. So the newest artificial heart doesn’t imitate the cardiac muscle at all. Instead, it whirs like a little propeller, pushing blood through the body at a steady rate. After 500 million years of evolution accustoming the human body to blood moving through us in spurts, a pulse may not be necessary. That, in any case, is the point of view of the 50-odd calves, and no fewer than three human beings, who have gotten along just fine with their blood coursing through them as evenly as Freon through an air conditioner.
“His giant heartbeat,” Rainer Maria Rilke wrote of God early in the past century, “is diverted in us into little pulses.” Nowadays, maybe not.

Home Made
The Texas Medical Center is a city within a city. Its 13 hospitals and 21 schools cover a swath of Houston bigger than New York’s Central Park. Navigating its raised sidewalks, light rail and glass towers feels like getting lost on a set for The Jetsons. One hundred thousand people work and study here every day. The place has its own zip code.
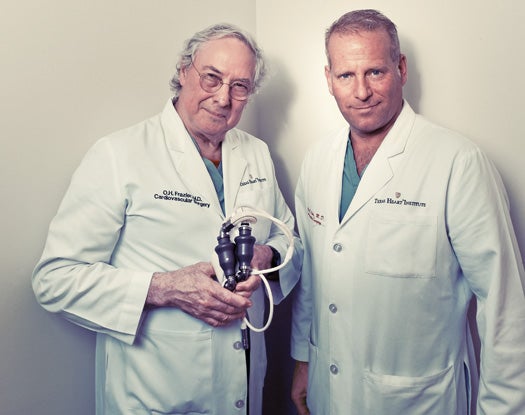
Among the towers is the Texas Heart Institute, in which I found Dr. Billy Cohn, a big, fit man in his early 50s with light hair, blue eyes, and an office that would no doubt have exasperated his mother. It looked like the mad scientists’ club at a middle school, every surface covered with sketches, tools, bits of machined metal, wire, statuettes, playing cards and such toys as a Darwinian evolution action-figure set (horseshoe crab, various monkeys and a gray-bearded intellectual). A static-electricity generator flashed lightning bolts, and a three-dimensional model of the human heart loomed over Cohn’s desk. Even his file cabinet looked weird, pimpled with tiny bits of metal.
“Rare-earth magnets!” Cohn cried, straining to pull one free. He put it in my hand. It was the size of a pencil eraser, and when I loosened my grip, it shot like a bullet to the file cabinet with a clang. “Extremely powerful.” Cohn has pioneered the use of rare-earth magnets to move catheters into place deep inside the body. He avoids having to cut patients open by threading the magnets, and their tiny loads, up through arteries. He pawed several sheets of paper off the floor and drew diagrams on their unused backs, launching an hour-long discourse on the instruments and procedures he’s built around miniature magnets.
Building a heart that mimics nature’s lub-dub may be as comically shortsighted as Leonardo Da Vinci designing a flying machine with flapping wings.On his wall hung four metal serving spoons of the kind you might see on a cafeteria line. One was intact; the other three had intricate slots cut in them. Years ago, Cohn butchered the spoons in his home garage to solve the problem of holding a heart still while operating on it. The standard way, at the time, was to shut off the heart altogether and put the patient on a heart-lung machine. But that was risky. Cohn’s spoons let surgeons hold a heart in place while still giving them access to the parts they needed to slice or stitch. Through the custom-cut slots, the surface of the heart would emerge and hold still for tinkering, even while the rest of the heart thrashed around under the spoon. Cohn refined the idea and sold it to a medical-devices company, which has marketed the tools worldwide.
Cohn grew up building rockets in the garage with his older brother John, and neither of them ever quite outgrew it. (John is one of 80 IBM fellows, the company’s highest technical rank.) “That there?” Billy Cohn said, pointing to what I’d thought was a scuba diver’s speargun. It hung on the wall beside laminated newspaper clippings about him. “I invented that out of old parts in the garage. It puts a bag, like a big sock, all the way around the heart.” He spent 20 breathless minutes describing why a surgeon would want to do such a thing.
It’s the continuous-flow artificial heart Cohn installed in the chest of Meeko the calf, though, that enthralls him now. Using such turbines to assist sick hearts has been standard practice since the mid-1990s. But along with his research partner, Dr. O.H. “Bud” Frazier, Cohn is experimenting with using them to replace the heart entirely—and doing so with the hands-on ingenuity of the professor on Gilligan’s Island. He rummaged through the detritus on his desk and placed in my hands two gray metal cylinders—turbines, each the size and shape of a saltshaker—connected to each other by white tubing. Also attached to each was a white cone made of a spongy rubberized cloth.
“Dacron polyester,” he said. Because the cones are what get sewn to the remainder of the heart’s atria, their design was tricky. He ticked off the concerns on his long fingers. “The materials needed to be blood-friendly. The structure needed to be resilient to deformation. It had to be formable in a limited space. We needed to be able to sew it, but the needle holes couldn’t let blood leak. And we had to be able to customize it in the OR by cutting it. I bought some ordinary Dacron from the fabric store and RTV silicone from Home Depot to impregnate the outside. I did all this in my garage. My wife calls them dolly dresses.”
The continuous-flow heart solves the biggest problem with artificial hearts: longevity. One little turbine like the ones Cohn showed me has been running continuously in a lab for eight years and shows no sign of wearing out. Another advantage is that it runs on a battery no bigger than a videocassette. The patient can wear it in a kind of shoulder holster—cumbersome, but not as bad as sitting day and night beside a hissing compressor the size of a dishwasher.
It all made sense in theory, sitting in Billy Cohn’s office. But the whole idea of life without a pulse was a little too weird for me to grasp. It seemed like some sort of parlor trick. How could someone be alive without exhibiting the most fundamental sign of life? And how did anybody even dream up such a thing?
Two Hearts
The dire need for a practical artificial heart hit Bud Frazier like a thunderclap one awful night in the 1960s. An eager medical student, Frazier had watched the legendary heart surgeon Michael DeBakey open the chest of a 24-year-old man and install a new heart valve. Later that night, the man’s heart stopped. It was up to Frazier to reach in, grab the warm but flaccid heart, and massage it with his hand to keep the blood pumping. As long as Frazier kept opening and closing his hand around the man’s heart, the man stayed alive. And Frazier was highly motivated to continue. The man’s eyes were open and looking right at him.
Today, Frazier is a white-haired eminence at the Texas Heart Institute, as calm, soft-spoken and slow-moving as his partner Cohn is loud and speedy. “DeBakey finally told me ‘Stop,’ ” Frazier recalled. ” ‘We can’t save him.’ The chief resident said the same thing; told me to quit. I didn’t want to stop. I had the boy’s eyes right on mine. Finally, I stopped, and he died. I thought, ‘My god, if I can do that with my hand, we must be able to develop something we can pull off a shelf.’ “
For Richard Wampler, the road to the continuous-flow heart began in 1976 in the Egyptian village of El Bayad. Wampler, a surgeon and engineer whose passion is medical devices, was in Egypt volunteering on a medical mission, watching villagers use an Archimedes’ screw to pump water from a well. The screw, named for its third-century-B.C. inventor, is a simple auger in a pipe. As it turns, it lifts liquid with it. The image of that village well never left him. Less than a decade later, Wampler patented a device to move blood through the body, without a pulse, using an Archimedes’ screw. (“My experience with creativity is like that,” he told me on the phone. “I’ll be jogging or lying in the pool, and it will come to me.”)
“As long as Bud Frazier kept opening and closing his hand around the man’s heart, the man stayed alive.”
Wampler brought a prototype of his idea to Frazier, who was by now a renowned heart surgeon. It was the early 1980s, and the hot idea in heart surgery was to install a small pump in the chest, not to replace the heart but to assist the left ventricle in pushing blood throughout the body. (The work of the right ventricle—pushing blood to the lungs to be reoxygenated—was left to the natural heart.) Used that way, the pump was called a left-ventricle assist device, or LVAD. The problem was that the patient still had to be hooked up to a cumbersome compressor, and, because the LVAD pulsed like a heart, it wore out relatively quickly. Frazier and Wampler thought the Archimedes’ screw might prove to be a longer-term and more comfortable solution.
Most people in the cardiac-surgery world were skeptical. The International Society for Heart & Lung Transplantation’s journal turned down Frazier’s paper, saying (as Frazier recalled) that this was of some interest to Dr. Frazier but of no interest to the general clinical population and will have no impact on the treatment of heart failure. Sitting in his majestic, book-lined office, Frazier flapped a hand contemptuously. “I was like Robinson Crusoe doing magic tricks for the goats.”
But he’d pressed on. The most foreseeable problem with using an Archimedes’ screw to move blood, in his view, was damaging the blood itself. The most a person can tolerate is one shredded cell in 200,000. The continuous-flow turbine, spinning like a blender on high speed, seemed likely to tear the red cells apart. There was only one way to find out.
Frazier began implanting continuous-flow pumps, based on the Archimedes’ screw, in calves—not as complete artificial hearts, only as assists to the left ventricle. They were crude, the screw inside the animal connected by a spinning cable to a motor outside. It wouldn’t be anything a human would want, but it proved that the concept could work; the turbine did no damage to the blood—perhaps, Frazier theorized, because it shot the blood cells through so fast.
While Frazier was installing left-ventricle pumps in calves, a NASA engineer named David Saucier received a heart transplant from Frazier’s old mentor Dr. DeBakey. On follow-up visits to DeBakey at the Texas Heart Institute, the engineer became acquainted with Frazier’s project, and it got him thinking. Years before, Saucier had worked on the space shuttle, helping to put together the pumps that fed propellant to the main engine. Perhaps there were features of the pump that could inform the design of a better blood pump, one that wouldn’t need to connect to an outside motor.
Saucier got NASA to open an investigation in conjunction with Baylor College of Medicine, which is part of the Texas Medical Center. Squeezing the screw and the motor into a package small enough to fit in a person’s chest proved to be a knotty problem. When it wasn’t going well, one of the doctors cracked to a NASA engineer, “If you can send a man to the moon, then why can’t you make a blood pump?” The engineer replied, “They gave us a hell of a lot more money to send a man to the moon.”

Flow State 2
In 1995, 11 years after Saucier started NASA’s informal work on an implantable continuous-flow blood pump, some of the NASA and Baylor researchers helped create a company called MicroMed to bring the pump to market, and three years later, surgeons implanted one in a patient in Europe. (The FDA hadn’t yet approved it for use in the U.S.) By now, MicroMed had competition from a company called Thoratec, which had an Archimedes’-screw continuous-flow blood pump of its own moving through the FDA approval process. Eager to stay ahead, MicroMed made the bubble-era mistake of letting itself be acquired by a hedge fund called Absolute Capital Management, which starved the project as it imploded spectacularly, its principals facing charges of fraud. Thoratec zoomed past the wreckage of MicroMed and was soon testing its own device, the HeartMate II, in clinical trials.
The HeartMate II was an Archimedes’ screw with magnets implanted in the axle and an electric coil in the cylindrical case surrounding it—the saltshaker-shaped device that Cohn had placed in my hands. A charge zipped around the coil, drawing the screw along at 8,000 to 12,000 revolutions per minute. The axle spun on a synthetic-ruby bearing, lubricated by the blood itself. Connected to a portable battery, it let patients live fairly normal lives and was designed to stay in place forever, not merely as a “bridge to transplant.” Patients’ own hearts still worked; the continuous flow of the pump just helped things along.
And here’s where the story gets spooky. In November 2003, Frazier installed the newly approved HeartMate II to assist the failing heart of a young man from Central America who barely spoke English. His family members spoke none. So none of them fully understood Frazier’s instructions to return to the hospital frequently for follow-up. The young man walked out of the hospital and disappeared.
When he finally showed up eight months later, Frazier held a stethoscope to his chest and was stunned to hear no heartbeat at all. None. Even more-sensitive instruments would have found nothing resembling a pulse. The young man’s heart continued to flutter weakly, but it had effectively shut down. Although the HeartMate II had been designed to assist the heart, not replace it, in this case it seemed to be doing all the work: not just helping the left ventricle push oxygenated blood to the body, but pushing the blood hard enough to flow through the body, then back through the useless heart to the lungs, through the useless heart again, and into the pump to complete the loop and begin the process all over again. The reason the young man had never come back for follow-up, he told Frazier, was that he’d felt perfectly fine.
Thoratec won FDA approval of the HeartMate II in 2008, and surgeons have now installed continuous-flow LVADs alongside the hearts of some 11,000 people worldwide (among them former vice president Dick Cheney). But cases like that of the Central American man remain extremely rare. Newspapers reported that Cheney had no pulse, but in fact he and most other recipients continue to experience, as Cohn describes it, “cyclic fluctuations of pressure with each heartbeat.” Even though such fluctuations might be detectable only by an intra-arterial monitoring line hooked to a pressure transducer, they remain present. Patients walk around with videocassette-size batteries hanging under their armpits, their hearts still beating. Frazier, who invited Billy Cohn to join him at the Texas Heart Institute in 2004, has installed many LVADs. He showed me a video of one of his patients playing basketball and another participating in a hip-hop dance contest.
One of the most surprising things about the LVAD is that it does something the medical community had thought impossible: It reverses heart failure. Until the past few years, damage to the heart was thought to be permanent. But it seems that by relieving strain, an LVAD lets some hearts damaged by, for instance, heart attacks repair wall tissue and grow healthy again. Often the LVAD can be removed. “It’s like putting a cast on a broken ankle,” Cohn says. “You take it off when it’s healed. We had no idea that could happen.”
Some hearts, though, can’t be healed. And for those who continue to worsen even with an LVAD, the only choices are the increasingly hard-to-come-by transplant, or replacement with a machine. The experience of Frazier’s Central American patient told Frazier and Cohn that it was theoretically possible to replace hearts entirely with continuous-flow pumps. But that raised the kind of questions nobody had ever before had to consider. Our bodies have evolved to have blood move through us in pulses. Was a pulse necessary for reasons we couldn’t yet imagine? One possible snag that occurred to Cohn was the lymphatic system. Unlike blood, the ducts that move lymph through the body have no motor of their own. They surround arteries and get their motion from the pulse of the blood. “It was a good theory,” Cohn laughs. “So far, though, we haven’t found any evidence that continuous flow creates problems with the lymph.”

Cohn knows this because a few people, like Frazier’s Central American patient, do continue to walk around with no pulse at all. Describing a miracle patient he wanted me to meet, Richard Wampler told me that Rahel Elmer Reger had a functionally inert “stone heart” yet was living comfortably in upstate New York. I got on a plane.
Reger was 36 years old, a mother of two- and five-year-old girls, when she finally consented to have her heart valve replaced in 2009. She’d had no symptoms, but her cardiologist said the heart murmur she’d had since childhood really should be fixed. Her aortic valve, if left untreated, could someday seal up altogether. So Reger cleared her calendar and checked into Strong Memorial Hospital in Rochester, New York, thinking she’d be laid up for seven to 10 days.
Neither she nor her doctors know exactly what went wrong, but for some reason her heart wouldn’t restart after the surgery. She stayed on a heart-lung machine for an extremely damaging 14 hours. “Prepare yourself for your wife never to leave the hospital,” the surgeon told her husband, Tim, adding, with all the delicacy for which heart surgeons are renowned, “Now I’m going to get some soup.” By the time Tim saw his wife, in an intensive-care room so crammed with electronics that it looked like a discount store, she was being kept alive by two Thoratec CentriMags—big centrifugal pumps operating outside her body. From the looks of things, she wasn’t going anywhere anytime soon.
When Reger developed dangerous clots, the surgeon disconnected the left external pump and inserted a HeartMate II into her chest. She reacted well, and eventually they also disconnected the right-side external pump. Her own heart had never restarted—it lay in her chest almost completely still—but the HeartMate II seemed to be powerful enough to move her blood throughout her body. Seventy-two days after checking in for what she thought would be a week’s hospitalization, Reger went home to her daughters without a pulse.
I met her one drippy morning at her home in Clinton, a Norman Rockwell–perfect town outside Utica. Her husband is the Episcopal priest in town, and they were living in the yellow-painted rectory beside the 19th-century church. I expected Reger to look sickly, so when the door was opened by a vigorous, pink-cheeked woman of small stature yet big personality, I figured she was a nurse or a friend. Reger stood only five feet tall but had a piercing stare and a strong voice utterly unaccented by her Swiss-German childhood. She shook my hand firmly and led me inside. On her back, she wore a small quilted backpack; a cable ran from it and up her shirt.
“I remember going in and out that first day, and when Tim told me my family was coming from Switzerland, I knew it wasn’t good,” she said as we sat in a warm living room decorated with her daughters’ artwork. She extended her wrist for me to hold. It was warm, but might otherwise have been that of a dead woman: no pulse.
Reger’s heart doesn’t seem to be getting better, but it could hardly get worse. Like the heart of Frazier’s Central American patient, Reger’s has all but given up. Logically, she should be dead. Instead, she feels fine, caring for her daughters and walking a pedometer-measured two miles a day. So far, living without a pulse has caused no problems with her lymph or anything else.
A few people continue to walk around with no pulse at all. One of them was living comfortably in upstate New York
The little quilted backpack held two lithium-ion batteries and the HeartMate II’s computerized controller, which are connected by cable through a hole in Reger’s side. Needless to say, she has never left her backpack on a bus. “My cousin once disconnected me, though, by mistake,” she said. “I was showing her how to change the battery. She disconnected one, and then—I was distracted for a second—the other. I yelled, ‘You can’t do that!’ and then passed out. The device blares at you. She reconnected it, and I came back. I was probably out for 10 seconds. She was completely freaked out. She wanted to go right back to Switzerland.”
Reger and the Central American patient proved that humans could survive, indeed thrive, with no pulse. But Frazier and Cohn were attempting to achieve intentionally what those patients had done inadvertently. Rather than augmenting an existing heart, which may lack sufficient strength and is in any case full of crannies that can grow dangerous clots, they would replace it entirely with two turbines, one to do the work of the left ventricle and one to do the work of the right.
Last March, they got their long-awaited chance. A 55-year-old man named Craig Lewis showed up at the Texas Heart Institute with a case of amyloidosis, an extremely rare and severe condition in which the body produces a rogue protein that gradually fills the organs with what Cohn calls “an insoluble muck.” Lewis had slid from perfect health to death’s door in less than a year.
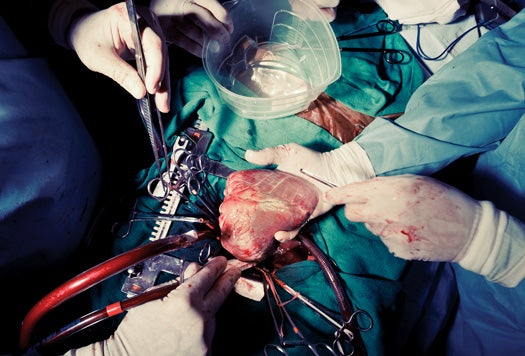
The doctors attached him to a heart-lung machine, and another device took over the function of the kidneys. He kept going into cardiac arrest, though, and staying attached to the machines was no longer feasible in any case. “That’s permissible for only five days, and he was on day 14,” Cohn says. “That’s when we started thinking about our device. There was no way he would have survived a heart transplant; the amyloid would have attacked it.” Lewis knew he didn’t have much choice and decided to give the turbine a shot. Cohn removed Lewis’s diseased heart and replaced it with a pair of HeartMate IIs.
Two days after surgery, Lewis sat up in bed and spoke with his family. An aspiring engineer, he even sketched ideas for how better to hook up the heart. Cohn showed me a photo of him drawing diagrams on a pad. The patient’s liver failure from the amyloidosis was so bad that within five weeks, he lost consciousness and his family asked Cohn to switch the heart off. But he’d gotten those five weeks—time to say goodbye. And he’d left a legacy. In those five weeks, Frazier and Cohn had proved that two tiny, continuous-flow turbines could replace a natural heart.

When Cohn and I entered the operating room, all we could see of Meeko was a tall mound of blue surgical drapes and a red rectangular cavern: Meeko’s chest cavity. Other surgeons had prepped the calf for surgery. Cohn was stepping in, as usual, to work the final miracle.
Twenty-eight people attended—technicians running the heart-lung machine, anesthesiologists, veterinarians of various stripe, photographers and goggle-eyed medical students. Everybody was walking around and talking; it was like a big cocktail party, only the guests wore scrubs and all you could see above their masks were their eyes. Among the guests was Bryan Lynch of MicroMed, the hedge-fund-wrecked company, now risen from the dead. Lynch and a few others from the company’s early days had bought their company back from the debris of Absolute Capital Management for a net outlay of $2 million—pennies on the dollar—and had a design that put the magnets in the blades of the screw instead of the axle. That shrunk the axle and made the blades bigger, which meant the screw could turn more evenly. That and a new silica-carbide bearing, Lynch hoped, would reduce the risk of creating dangerous blood clots. It was MicroMed’s pumps that Cohn was preparing to implant in Meeko’s chest.
Overhead, a big flat-screen TV, connected to a miniature camera on Cohn’s forehead, gave us a surgeon’s view of the procedure. The medical students gazed at it raptly. I didn’t use it because Cohn had told me to stand at his left elbow, where I could peer straight down onto the calf’s red, thrashing heart.
Working with an electric cauterizing scalpel that sizzled as it touched flesh (and sent up a distinct steakhouse aroma), Cohn peeled tissue from around the heart. The more its constraints were peeled away, the more vigorously the heart seemed to buck. “Go on!” Cohn yelled, which was the signal for the heart-lung machine to take over. A thick transparent tube filled with dark, purple blood from the calf, and another tube returned it a livid red. With a few deep, swift strokes, Cohn cut the heart free and lifted it on his palm. He left the atria of the heart—a sort of lid, where the big vein and artery go in and out—inside Meeko’s chest. The rest of it continued to beat as he laid it in a basin because residues of blood remained in the small coronary arteries. Cohn cocked an eye at me over his mask. “I’ll bet you’re thinking, ‘How dare he.’ ” Actually, what I was thinking was: Thus begins my life as a vegetarian.
Working fast, Cohn sewed collars of rubberized Dacron onto the atria. His stitching looked like plain old needle-and-thread work, low-tech and almost casual in its rapidity. Within a few minutes, he had fixed in place two white, doughnut-shaped collars. He lifted the turbines from a dish of saline, their rubberized-Dacron dolly dresses dangled from them. They were marked “Not Approved for Human Use,” but each was smaller than the HeartMate II, another advantage MicroMed hopes one day to exploit.
Working as deftly as ever, Cohn sewed the dolly dresses onto the collars he’d installed in the atria. There was no dramatic moment when the turbines were activated and the heart-lung machine turned off; it happened sometime during the third hour of surgery. But at one point, I noticed that the blood-pressure monitor no longer displayed two numbers—120 over 80—but one: 78. “Usually we measure blood pressure at the moment the heart squeezes and the moment it relaxes, the systolic and diastolic numbers. This calf has only one now. And check out the pulse.”
Flatline. William Shakespeare, many scholars believe, wrote sonnets in iambic pentameter to imitate the sound of a human heartbeat. What, I wondered, would the Bard make of this?
Cohn kept freaking me out doing magic tricks. In the elevator on our way upstairs from the operating room, he pulled five one-dollar bills from his pocket. “Five singles, right?” he said. He turned the bills over in his hand and swiveled the palm upward with a flourish. The five ones had turned into five 100s. There was nothing up his sleeve; he still had on his short-sleeved scrubs.
Back in his office, he asked me to pick a card at random from a deck, look at it, and put it back in the deck. It was the 10 of diamonds. He told me to draw a shape in the air with my finger. I drew a triangle. “Think of a color but don’t tell me what it is,” he said. I thought of green. He cut the deck, and there was the 10 of diamonds, a green triangle inked on it. I almost passed out.
It wasn’t until that evening, when we sat in a windowless break room drinking terrible coffee, that he revealed why he’d kept showing me magic tricks—to refute, in a way, Arthur C. Clarke’s famous dictum, that advanced technology is “indistinguishable from magic.” First, though, Cohn set aside his coffee and cracked his knuckles. “Now,” he said in a P.T. Barnum voice, “I’ll show you the amazing disappearing saltshaker. Usually I do this with a special silk, but . . .” He looked around, grabbed a stiff brown paper towel, shrugged, and wrapped the plastic shaker in it. “No, wait,” he said, the smoothness of his act ruined. “This is the amazing saltshaker-through-the-table.” He set the wrapped saltshaker down on the table with a loud clunk, stopped, took it away, and said, “Sorry. Maybe it’ll work better with these.” He put some packets of pepper on the table, thought a second, and then swept them away. Something had him rattled, I couldn’t tell what. “No, it’s the saltshaker. That’s right.” He set it up on the table again with one hand and smacked it hard with his palm. The paper towel flattened out, and we heard the saltshaker bounce off the floor below the table. I bent to retrieve it, flummoxed.
“OK,” he said gently. “Let me deconstruct it for you.” All those fumbling mistakes with the silk and the pepper packets were, as it turned out, part of the trick, designed to distract me from what was really going on: his molding the stiff paper towel to the saltshaker and secreting the shaker under the table. When he smacked down the towel, he released the shaker, which he’d been holding under the table. “It’s all part of a script. Every word I said, every motion of my hands, had a role in making the trick work. It seemed random—even like mistakes—to you. But it was all part of the script.”
He sat back and spread his hands. “That’s what heart surgery is,” he said with a soft laugh. “It’s a script. To you, it probably looked like I was just sewing those collars into Meeko’s chest any old way. But every motion was planned, tested, practiced. Turn my hand eight degrees and poke the needle through; swivel my hand back 22 degrees and draw the needle up four inches; turn my hand back just so and bring it to the left a half inch: a precise number of stitches, pulled just so tight and no tighter. What heart surgery takes is remembering an incredibly long and complicated script and following it exactly, step by step.”
Walking back to his office, I pressed him on how long it would be before people were walking around with continuous-flow artificial hearts. Some people think that pressure from the medical-equipment industry makes the FDA too hasty in approving new medical devices. Others think the opposite—that pressure from the insurance industry makes the FDA drag its feet, because insurance companies don’t want to pay for expensive new therapies or, god forbid, keep deathly ill people alive longer. Cohn was in neither camp. “They have a hard job to do, and we want them to be careful,” he said as we sat down again amidst his playing cards and heart models. Besides, the technology really isn’t ready, he said. Using two turbines, with two computerized controllers, is cumbersome. “It really needs to be one integrated unit.” That will take another three or four years to develop, he estimated, and then another six or seven for the trials necessary for FDA approval. But the principle has been proven, he thinks. The delay didn’t bother him; it’s part of scientific advancement: “The Wright brothers flew 800 feet in 1903, and commercial air travel began in 1920.”
“Oh, hey! Look at this,” he suddenly cried, pawing through the mess on his desk. He came up with a small cardboard box. On the lid, he’d pasted a photograph of the continuous-flow artificial heart, and below it, the letters S, M, L and XL. He’d circled the L with a red Sharpie. “Doesn’t that look cool?” he said, holding it up for me to admire. It looked like a novelty item you’d pick up at a magicians’ supply store. “It’s a joke,” he said, “but this is kind of what I envision. That you’ll be able to walk into Costco, pull this off a shelf, and have your surgeon stick it in your chest. These things are so simple, we’ll be putting them in the chests of 100,000 people a year.” He set down the box, picked up the turbines with their dolly dresses, and turned them over lovingly in his hands. Just as human flight wasn’t possible until people gave up the idea of imitating birds, permanently replacing the most vital of organs may not be possible without ridding our minds of the heart’s telltale beat. “I think we’re on the verge, right now, of solving the artificial-heart problem for good,” he said. “All we had to do was get rid of the pulse.”
Dan Baum is the author, most recently, of the book Nine Lives:Mystery, Magic, Death and Life in New Orleans.
Check out more from our Future of Medicine issue here.
In a previous version of this article, the author implied that a heartbeat’s lub sound signifies blood being sent to the lungs, and that its dub sound corresponds to blood being sent to the body. This is not correct. The blood is sent to the lungs and the body at the same time, from two separate ventricles, on the dub part of lub-dub.
Join Our Telegram Group : Salvation & Prosperity