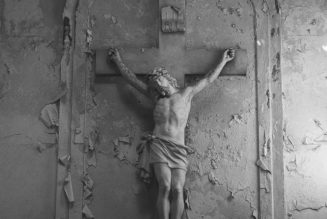
Floridians doing the right thing.
Sam Greenwood/Getty Images
Slate is making its coronavirus coverage free for all readers. Subscribe to support our journalism. Start your free trial.
The past week’s tiny anti-lockdown protests are the exception that proves the rule: The U.S. has demonstrated widespread commitment to quarantine, social distancing, and business closures to stop the spread of the coronavirus. The response has surprised some skeptics who predicted that true patriots would never stop going to Applebee’s, and it raises the possibility that even Americans might submit to the mass test-and-trace programs that are underway in South Korea and on the way in Germany, two countries that appear to be handling the pandemic well.
Maybe that’s not so surprising. With its promise of atonement through drudgery, home confinement taps into that puritanical strain of American culture that H. L. Mencken described as “the haunting fear that someone, somewhere may be happy.” That quip perfectly captures the angry reaction to Jacksonville, Florida’s decision to reopen its beaches on Friday afternoon to activities like biking, fishing, running, swimming, and surfing. (Sunbathing, organized sports, chairs, coolers, and grills are not allowed.) People in Jacksonville might have been happy, but people everywhere else were mad.
It was hard to separate the scenes of Jacksonville beachgoers from several compounding factors: Florida’s reputation for wild behavior, the reluctance of Trump toady and Florida Gov. Ron DeSantis to close restaurants and bars during spring break as the coronavirus swept the nation, and the ill-advised plans in neighboring Georgia to open most of the state’s businesses by Monday. But try if you can: On Friday, Jacksonville was tapping its biggest public space for limited, socially distant use.
Good idea, and it would be a good idea most anywhere right now. Until we are able to halt widespread community transmission and begin testing and contact tracing, it’s too soon to “reopen” the economy in the way Donald Trump envisions. But we can get more Americans—and even businesses—safely outdoors.
Those Florida beaches aren’t so different from Central and Prospect parks in New York City. Frederick Law Olmsted’s two “green lungs,” the American city’s quintessential public health infrastructure, are offering New Yorkers critical physical and mental respite during their city’s darkest hour. And why not?
“I would not worry about walking by someone,” said Dr. Amesh Adalja, an infectious disease specialist at Johns Hopkins University. “Even in a health care setting, contact is defined by being near someone for a certain amount of time. I would not worry about these fleeting encounters. The virus isn’t airborne—droplets need to get from one person to another.”
We can get more Americans—and even businesses—safely outdoors.
The issue, Adalja added, is that beaches tend to be places where people don’t keep their distance. Any additional open spaces where people interact even in passing, he added, create the potential for new cases.
But what little we know about the coronavirus suggests you have little to fear from brief encounters with other human beings outside. Dr. Edward Nardell, an airborne-infection specialist at the Harvard T.H. Chan School of Public Health, said outdoor transmission was “possible but improbable.”
“It bugs me to see these restrictions on people being outside,” Nardell said. “Mental health means something as well, and I can’t imagine you’re in a better place than outside if you’re going to have any contact anywhere.” Nardell, who survived a recent battle with COVID-19, said that if he were in Massachusetts Gov. Charlie Baker’s shoes, he would go ahead with opening the state’s beaches—but with strong signage reminding people to keep their distance and under park ranger supervision.
Nardell’s colleague Marc Lipsitch, an epidemiologist, wrote a more general case for public spaces in the Washington Post last week.* “Closing parks and public gardens should be a temporary, last-resort measure for disease control,” he and his co-authors wrote. “The science could not be clearer: The benefits of getting outside vastly outweigh the risk of getting infected in a park.” Wear a mask, keep your distance, have a ball.
In many U.S. cities, though, the largest public spaces are still closed. Those include beaches across Southern California, the Lake Michigan waterfront in Chicago, and the National Arboretum in D.C. These closures were motivated by sincere public health concerns, but they have had the effect of punishing city residents who don’t have access to country houses or private green space to relax. And it’s not clear they do much good.
Several news stories helped raised the alarm about how COVID-19 might be transmitted outdoors. In a popular story in the Atlantic last month, a doctor warned a mother not to ride a bike through New York City: “You rode a bike? With viral load everywhere? Why?” Some widely shared bullshit out of Belgium suggesting runners stay 65 feet away from each other. A more respectable piece in the Journal of the American Medical Association suggested that “pathogen-bearing droplets of all sizes can travel 23 to 27 feet.” But that was a model, not real life.
“A single virus particle could get you sick theoretically,” said Dylan Morris, a Ph.D. candidate at Princeton who studies viruses and was part of a group that researched how COVID-19 could linger on surfaces and in the air. “But that’s a slightly misleading picture. How much virus do you have to encounter in practice to have a 50 percent chance of getting sick? It may take orders of magnitude more than one. Hundreds, thousands, before you’re at serious risk of infection.” That is reason to focus more on high-risk encounters, as in health care settings, than on low-risk ones—like passing someone on a bike path.
“I’m a runner, and I wouldn’t feel that guilty about accidentally getting slightly close to people,” Morris added.
Disease scientists have been engaged in a mostly semantic dispute about how the coronavirus spreads. The current consensus is that it can be transmitted indoors, by asymptomatic people, across substantial distances. This is what apparently happened to a choir in Washington state, where 60 singers gathered in early March but (they later said) kept their distance. Four weeks later, 45 had contracted COVID-19. Two are now dead.
In a paper to be published in a Centers for Disease Control and Prevention journal this summer, Chinese researchers studied a restaurant in Guangzhou where one diner seems to have passed the disease to five patrons at neighboring tables (and four at her own) in the 1,500-square-foot dining room. The three infected tables all lay in the path of a wall-mounted air conditioner, and all the guests overlapped for about an hour. Ten people at those three tables were not infected, and neither were any of the 73 diners in the rest of the room.
Whether that qualifies as good news about the limits of indoor transmission or bad news about restaurants depends on your point of view.
But infectious disease specialists say there is a big difference between indoor and outdoor air. Outside, germs simultaneously dilute and decay. Tuberculosis, for example, is caused by highly contagious bacteria. But, says Nardell, “I’m not aware ever of a report of tuberculosis being spread outdoors.”
Wear a mask, keep your distance, have a ball.
COVID-19 is not tuberculosis; we don’t yet know how it moves in air or how much viral exposure sickens people. Still, a handful of studies point to encouraging news about outdoor transmission risks. Scientists in Wuhan tested the air at various public sites around the city in February and found “undetectable or very low concentrations” of virus particles, except at two sites in front of a department store and a hospital. Even there, as Ed Yong observed, the concentration was many times below the threshold considered infectious for the original SARS virus of 2003.
In another preprint, Chinese researchers traced 300 outbreaks outside of Hubei province, using case reports from local health commissions between Jan. 4 and Feb. 11. (Hubei, which contains Wuhan, was not locked down until late January.) Eighty percent of outbreaks involved domestic transmission; 35 percent involved transport. One outbreak can involve multiple transmission venues. Out of more than 7,000 cases, the researchers found only one documented outdoor transmission: a man who got sick after a conversation outside with a man who had recently come back from Wuhan. All outbreaks involving three or more cases occurred inside.
“The transmission of respiratory infections such as SARS-CoV-2 from the infected to the susceptible,” the researchers conclude, “is an indoor phenomenon.”
Your mileage may vary with respect to Chinese data and preprints. “Almost everything we’ve been told is based on no data,” Nardell said. “No one can ever say, ‘This is safe.’ ” Opening public spaces will be a political decision, not one arrived at through medical consensus.
But it wouldn’t be the first outbreak where it helped to be outdoors: A study of open-air treatment during the 1918 influenza epidemic concluded, “A combination of fresh air, sunlight, scrupulous standards of hygiene, and reusable face masks appears to have substantially reduced deaths among some patients and infections among medical staff.”

Bicyclists in Brooklyn’s Prospect Park. You can do this!
Spencer Platt/Getty Images
The good news is that many American indoor spaces have outdoor equivalents. Crowded city apartments have parks and beaches nearby. Busy neighborhoods have streets that have been all but emptied of cars; many cities are transforming that asphalt into play space for children and exercise space for adults. And restaurants and shops have parking spaces in front that can, with just a little work, be appropriated to provide tables and chairs, or simply a well-ventilated space for pickups.
Not every city has a beach like Jacksonville. But every city has a big street that could be turned into an outdoor space for people: a promenade, or a dining area to allow cluttered restaurants to safely reopen when lockdowns and community transmission give way to testing and contact tracing. Underneath the paving stones, the beach.
Of course, officials are afraid that people will not follow best practices. (In some cases, this is why public spaces were closed in the first place.) An encouragement to go out would muddle a public health message focused on “stay inside.” Park- and beachgoers will talk with one another. They’ll flirt. They’ll build human pyramids at the water’s edge. In several cities, police have taken the responsibility to force people apart.
Is opening these public spaces a risk? Yes. “Social distancing goes down, infections go up,” says Adalja, the Johns Hopkins doctor.
But it’s a risk many infectious disease experts think is small compared with the certain damage we cause by keeping people inside. Regular exercise is as good as pharmaceuticals for reducing depression. Time in nature soothes ADHD symptoms in children and helps them concentrate. Being outside makes us less stressed. Just looking at the outdoors makes us more productive and less sick. And that doesn’t even reckon with the social tensions imposed on people quarantined with family, or the loneliness of those who live by themselves.
Moments of crowding do not warrant police intervention or park closures. On the contrary: They’re a sign that people desperately want to be outside, and that we should give them more places to go. We thought we might be facing a summer where we couldn’t go outside. From a public health perspective, it might be better to go out and stay there. Six feet apart.
Correction, April 23, 2020: This piece originally misspelled Marc Lipsitch’s first name.
For more COVID-19 coverage, listen to What Next.
Readers like you make our work possible. Help us continue to provide the reporting, commentary and criticism you won’t find anywhere else.